A team of biomaterials scientists and dentists at the UCLA School of Dentistry has developed a nanoparticle that, based on initial experiments in animals, could improve treatment for bone defects.
A paper describing the advance is published today in the journal Science Advances.
Bone defects, which can be caused by traumatic injury, infection, osteoporosis or the removal of tumors, are difficult for orthopedic surgeons to treat. And the need for bone grafts are becoming more common thanks in part to our aging population: Bone injuries are particularly prevalent among the elderly.
Today, the standard treatment for bone defects is a bone graft, which involves transplanting healthy bone from another part of the body to repair the damaged area. However, the procedure can cause complications, including infections where the transplanted bone is taken from, bleeding and nerve damage.
So the researchers turned their attention to liposomes, tiny spherical sacs that are derived from naturally existing lipids. Liposomes have been used since the 1990s to treat cancer and infectious diseases, and more recently they are being explored for their possible use in bone tissue engineering. They can be used to administer nutrients and pharmaceutical drugs in the body and can easily enter cells to administer their valuable cargo, but they do have some drawbacks: They are physically unstable and it can be difficult to control how and when they release drugs.
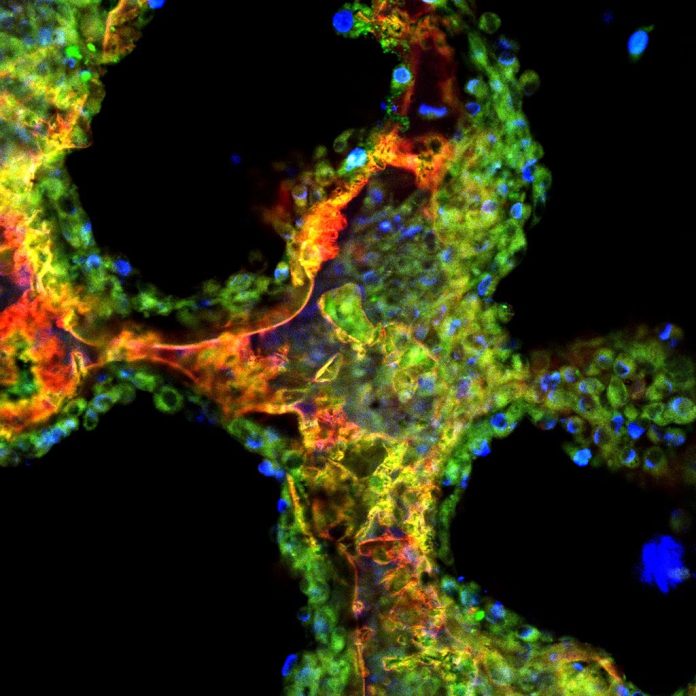
To help improve their stability and enhance their ability to form bone in the body, the UCLA researchers developed a new type of liposome called a sterosome. (The name is inspired by the fact that they contain a high concentration of steroids.)
To produce the sterosomes, the scientists replaced cholesterol, an important component of liposomes, with oxysterol, a type of cholesterol that has a key role in skeletal development and bone healing. In tests using mice with bone defects, the researchers found that the sterosomes successfully activated bone regeneration on their own, without needing therapeutic drugs.
“Liposomes are generally made from pharmacologically inactive substances,” said Min Lee, the paper’s corresponding author and a professor of biomaterials science at the dental school. “Including oxysterol into our liposomal formulation not only increased nanoparticle stability but also stimulated cells to develop into bone-forming cells.”
In a second phase of the study, the researchers wanted to see how they could make the sterosome even more effective.
They added their sterosome nanoparticle to a tissue engineering scaffold — a structure often used to move and grow naturally occurring stem cells, which is matched to the site of the defect and is used during bone graft procedures. They loaded the sterosomes with a bone-building drug called purmorphamine. Next, they immobilized the drug-loaded sterosome onto a scaffold to ensure that the sterosomes stayed concentrated in the defective areas and released the drugs where they were most needed for as long as possible.
In a six-week study using mice with bone defects in their skulls, the researchers saw an average reduction of roughly 50% in the size of the defects after the drug-loaded scaffold was implanted.
“By using our nanoparticle, which we found has intrinsic bone-forming capabilities, along with the addition of therapeutic drugs, we were able to speed up the bone regeneration process,” Lee said. “Our nanoparticle-packaged drugs will be useful in many clinical situations where bone grafting is required to treat non-healing skeletal defects and related bone pathologies.”
Dr. Paul H. Krebsbach, professor of periodontics and dean of the dental school, said, “The research led by Min Lee and his team demonstrates that UCLA Dentistry’s research endeavors go well beyond treating the diseases of the oral cavity, and their findings have wider implications for treating bone defects throughout the entire body.”
The study’s other authors are Chung-Sung Lee, Soyon Kim, Jiabing Fan, Hee Sook Hwang and Dr. Tara Aghaloo, all of UCLA.
The study was funded by the National Institute of Dental and Craniofacial Research, the U.S. Department of Defense and Musculoskeletal Transplant Foundation Biologics. The authors report no conflicts of interest.